As a caregiver, your child with cystinosis is your focus. But taking care of others may affect your own health. Your self-care may fall to the side. Do you get enough sleep, eat well, exercise, take breaks, and visit your own doctor? All of these may help keep you healthy so you can help care for someone with cystinosis.
Here are some things you can try to help relieve stress and stay healthy:
CAN is a nonprofit organization providing education, peer support, and resources to family caregivers across the country, free of charge.
FCA supports the important work of families caring for adult loved ones with chronic, disabling health conditions.
NAC is a nonprofit group of national organizations. It focuses on advancing family caregiving through research, innovation, and advocacy. NAC conducts research, does policy analysis, and works to increase public awareness of family caregiving issues.
RCI’s goal is to support caregivers—both family and professional—through advocacy, education, research, and service.
NORD, a nonprofit organization representing people living with rare diseases, has launched a program to provide caregivers of rare-disease patients relief. Financial assistance allows caregivers time away while ensuring their loved ones are well cared for.
A child with cystinosis may have needs or qualities that are different from their classmates. Sometimes, these differences can lead to social issues, like teasing, exclusion from peer-led activities, or bullying. While your child may never be bullied, it’s important to know it may happen and why your child may become a target.
Most bullying likely comes from a lack of understanding of cystinosis and what it means to live with a lifelong disease. So, education is key. Talking to teachers and other school staff can help them—and your child’s classmates—understand your child’s situation. Knowing that there are adults who can help may reassure your child when facing social issues. Educating your child may help, too. Knowing what to do if bullying occurs can help your child feel more comfortable and confident.
Help teachers and school staff understand the facts about cystinosis. Download this brochure and print it out to share in school, or email rareconnect@amgen.com to receive hard copies. You can also help your child’s classmates learn about cystinosis. Share Michael’s Activity Book with teachers so they can teach the students about cystinosis in the classroom.
Some things about cystinosis that may cause bullying at school include:
TEEN LINE is a nonprofit, community-based organization helping teenagers address their problems. The organization’s mission is to provide personal teen-to-teen education and support before problems become a crisis. TEEN LINE offers a national hotline you can call or text, and community outreach.
StopBullying.gov educates schools, kids, and parents about how bullying can happen anywhere, to anyone. With the right tools and information, everyone in the community can help stop bullying at school, online, and in the neighborhood.
PACER’s National Bullying Prevention Center actively leads social change so that bullying is no longer an accepted childhood rite of passage. PACER provides resources for students, parents, educators, and others. Bullying is a serious community issue that impacts education, physical and emotional health, and the safety and well-being of students.

Children with cystinosis want the same opportunities as any other child at school. They want to learn how to read, play at recess, and make friends. But sometimes the challenges of living with cystinosis may get in the way. Below are some tips to help you work with your child’s school so cystinosis is less likely to get in the way of your child’s experience.
Help teachers and school staff understand the facts about cystinosis.
Cystinosis may cause your child to miss school. The major reasons for absences may be:
If you know your child is going to be absent, be sure to tell the school and your child’s teacher in advance. You can even make a missed-school plan with your child’s teacher. This can help your child keep up with classwork during absences.
Helping peers understand cystinosis can make a big difference for your child. You, your child, or the school nurse may want to speak to teachers and students at the start of the school year to explain cystinosis to them.
This checklist contains helpful tips for making your child’s life more manageable at school. Work with your child’s school to complete this checklist.
Create a plan for managing your child’s medicine at school
Consider:
Identify a staff member to be your child’s go-to advocate
Ask your child’s teacher to make special arrangements to make the classroom more comfortable for your child
Consider asking if your child can:
Work with the school to create a plan for keeping up with schoolwork
You might want to:
Discuss how cystinosis affects your child’s participation in physical activities and/or recess
Plan what other students will be told about your child’s cystinosis
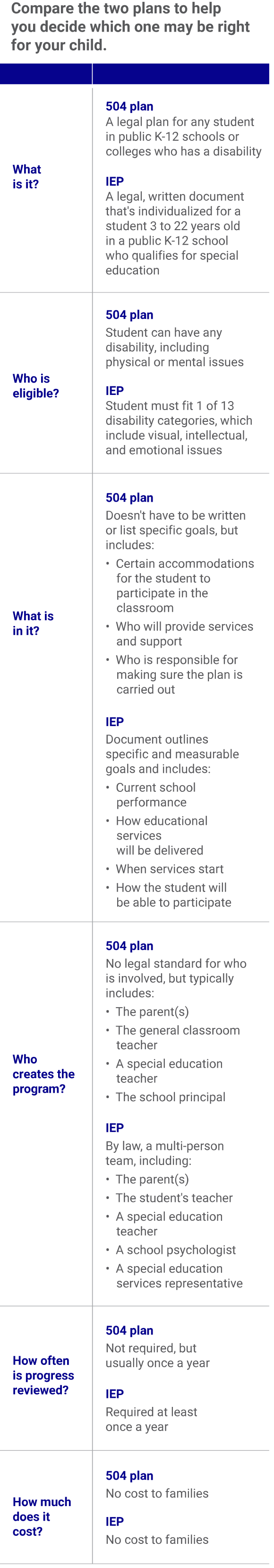
When a child has a complex disease such as cystinosis, it can be hard for teachers and school staff to understand. This is why there are special laws that allow a plan to be made for your child. These plans are called a 504 plan and an individualized education program (IEP).
These plans can help students living with cystinosis by:


The following downloadable and video resources are intended to provide tips and tools to help you face the daily challenges of cystinosis head on.
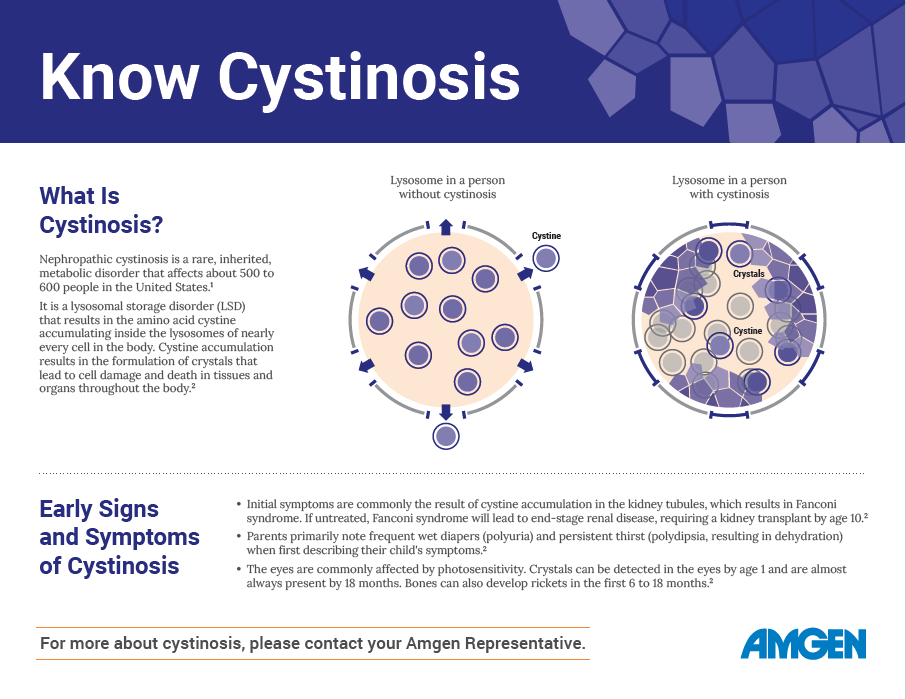
If you have questions about cystinosis, use this informational download to start a conversation with your child’s doctor. When you better understand cystinosis, you can educate those around you and build the network of support your child needs.
Whether you are getting ready for your first kidney transplant, or you have been through one before, use this guide to feel better prepared and informed.
Dialysis may become an important milestone in your cystinosis journey. Use this guide to feel better prepared and informed and get helpful ideas on how to stay positive.
Transitioning to adult health care is an important milestone in the cystinosis journey. There are things you can do to help navigate your transition, be responsible for yourself, and maintain independence.
Watch pediatric nephrologist Dr Ken Lieberman discuss critical issues like involving siblings, the best time to do white blood cell testing, involving children in their health care decisions, adequate nutrition, and more.
[DR LIEBERMAN] In a family where there are siblings of the child with cystinosis, I think it's very important that the parents bring that sibling into the discussion process to the degree that's developmentally appropriate early on. And the younger sibling or the older sibling’s going to be a companion for your child with cystinosis long into the future, and the sooner they feel involved and invested in this disease, I feel that the better that's going to go for everybody.
[DR LIEBERMAN] I find it very helpful that I have my patients go and do their periodic blood testing a week before their next visit with me, and I then have the results sitting in front of me. So, when they come in, I don't have to say, like, now go do your blood testing, but I have the results. And we can have a very worthwhile meeting, reviewing where we've been and what we have to do for the future.
[DR LIEBERMAN] Engage your child in making decisions about his or her health care day-to-day aspects as early as you can. The child may express that they want to take the meds an hour earlier or at this time as opposed to that time because their favorite TV show is on or something like that. Be flexible with them even relatively early on and let them have some control over their day-to-day care. Explain in an age-appropriate way that they are going to, that they are different in the sense that they are going to need to take responsibility for their health care that other children may not have to deal with.
[DR LIEBERMAN] It's easy to be overwhelmed by the enormity of this diagnosis and the implications for the future. And sometimes being overwhelmed by the big picture can lead to paralysis and make it difficult for you to address the everyday problems, not only of your child with cystinosis, but other problems within your family. The antidote to such a paralysis is focusing on the day-to-day. If you can do that, if you can focus on the day-to-day and carry forth with the things that you have to do, you will find the overwhelming thoughts that creep up to recede further and further into the background.
[DR LIEBERMAN] Consistency in the taking of the medication, which is so important in the treatment of this disease, is a major problem for families. The children go through phases of being perhaps more obstinate, and trying to break with a schedule that perhaps you had established for many years. Try to take into account the child's schedule. Ask him or her, what are the barriers? Why is medication-taking becoming a problem now? And encourage them to tell you what they see as the issues.
It may be something as simple as the timing of the administration of the medication, but try to see it from their angle and see if what they want can be addressed and validated. However, if you see the problem with medication-taking as escalating, bring it to the attention of your healthcare provider sooner rather than later so that you can have their assistance in trying to get things back on track.
[DR LIEBERMAN] For many of the families that I have been involved with, daily feeding is the biggest ongoing challenge for their young children. Feeding is very emotionally fraught. It cuts right to the center of what it means to be a nurturing parent, to be able to give your child good nutrition. And often these kids with cystinosis are not good eaters. And so, getting adequate nutrition into the patient is sometimes difficult. You need to overcome the sense that this is your failure. It is not; this is a problem of this disease. It needs to be seen in that light and it needs to be overcome. Your physician will be able to give you lots of tips and tricks about how to deal with giving adequate nutrition to these young children with cystinosis.
I have found, and many other experts in the field have found, that utilizing some form of direct stomach feeding NG tubes, gastric tubes, can be extremely helpful, almost liberating for the family. Again, it's seen as a surgical procedure or a medical procedure where a tube needs to be inserted to facilitate feeding. But then once that's done, you don't have this enormous day-to-day burden of sitting there with the spoon or the bottle and trying to coax your child into taking every spoonful. But you have a ready mechanism to ensure that your child is receiving nutrition that's adequate for their need. And this is definitely something that you would bring up with your physician to see if this might be appropriate for you.
[DR LIEBERMAN] Just like parents need to struggle with their children eventually leaving the nest and going out on their own, we pediatricians all have to struggle with the time when our children, our patients, your children are graduating from us and are making that transition from pediatric style medical care to adult style medical care. This is a discussion that you definitely have to have with your pediatrician. They might have very clear thoughts of their own about how to manage this and when to do various steps. College, which so many of our patients will be experiencing, forms a natural timeframe for some of these transition points. They transition to college, which if the college is not in the hometown, they're not living at home, forms a little bit of the transition and the college health facilities, the infirmaries, are often very helpful in doing that. But I think for most pediatricians, there's a relatively hard and fast transition point around the age of 22, when the children are graduating college. And we can help you find adult care for your child and help you with the steps of that transition.
[DR LIEBERMAN] There comes a time when your child, who perhaps is no longer such a little child, wants to know about the impact of cystinosis on their own life. Certainly, answer to the best of your ability any questions your child may come up with. But this is definitely a space where your health care provider could be of great assistance. The child should feel that he or she has a direct relationship with their doctor, not just through the parents. And the doctors will, in an age-appropriate way, answer questions about how this disease will affect the children as they get older. This requires some sensitivity to stage of development the way one would deal with this question, namely, the impact of the disease on my life, would be different with a 12-year-old versus an 18-year-old. But it's a discussion that needs to take place.


The self-care project is your guide to help you realize your full potential physically, mentally, and emotionally. Self-care is the best care. That’s why it’s important to challenge yourself by setting goals, improving your overall well-being, and finding motivation.
(for teachers and school staff)
Share this brochure at your child’s school to help teachers and school staff understand the facts about cystinosis and how the condition can impact students’ lives at school. They will learn how to support your student with cystinosis and educate other students about the disease.
Do you or your child ever get tired of explaining to others what cystinosis is and how it affects you? Here is a video called, “I Live with Cystinosis” you can share with others to do the explaining for you or your child!
Share video[MUSIC] Light, unobtrusive background music
[PATIENT] I live with cystinosis. It’s a rare genetic disorder affecting only about 500 to 600 people in the United States.
I am rare. And guess what? So are you! Not many people get to meet a person with cystinosis!
I want you to know about my symptoms and side effects that happen because of my disease and the medicine I take to treat it. Fortunately, cystinosis can be managed.
I experience sensitivity to light. Cystinosis causes cystine crystal formation in my eyes. I often wear sunglasses to help with the light.
I am sensitive to heat because cystinosis impairs my ability to sweat. I try not to be too active in warm rooms or when it’s hot outside.
I may have to miss out on things if I have doctor appointments, if I’m feeling sick, or when serious things come up and I have to go to the hospital.
I sometimes experience low energy levels. Snacking frequently during the day helps.
I sometimes experience near-constant thirst because cystinosis causes dehydration.
I carry a water bottle and I have to go to the bathroom frequently.
I know it’s really important for me to take my medicine. But sometimes the medicine causes me to have bad breath or body odor. I eat mints, chew gum, or apply essential oils to try to help.
I work hard to manage my disease and have since I was a little kid. It’s important that I take my medicine on time and I really try to never miss a dose. If you have any questions about what my life is like or what I am dealing with, please just ask! I want you to know about me and my life with cystinosis. Thank you for letting me share this with you.
I have cystinosis but it does not define me!
[AUDIO] Sound effect when the “i” is standing in front of final frame


Looking for a fun way for your child to learn more about cystinosis? Encourage your child to join Rapido the Sloth and Remmy the Robot on some fun adventures in a virtual reality experience designed to support them in their management of cystinosis.
This booklet for your teen with cystinosis provides tips needed to juggle life, school, friends and cystinosis. Here they will get information like the importance of keeping their muscles moving, things to bring with them when they go out, the right sunglasses for their face shape, and much more!
The Hangout is a place where your teens can go to help figure out life with and beyond cystinosis. They can get motivation, tips, and inspiration.
Join Ruby on her quest to find and remove cystinosis crystals throughout the body in this informative animated lesson for young children. Watch and discuss the video, then continue the discussion by ordering the Quest for Crystals book.
[Background music]
The Quest for Crystals writes on screen
[VO]
Meet Ruby
She’s an explorer. She searches for crystals in a surprising place.
The place where Ruby looks for crystals is in the body! She is like medicine that takes crystals out of the body. Travel with Ruby through the body to find as many crystals as you can.
Let’s go!
Crystals can be pretty and shiny.
But crystals don’t belong in your body. It’s good to get them out.
Ruby’s first stop is the kidneys. People are born with 2 kidneys.
Kidneys help your body keep stuff it needs, like water and salt, and get rid of stuff it doesn’t need.
But kidneys have a hard time keeping the good stuff in the body if they have crystals in them.
Help Ruby find a crystal.
Do you know how kidneys get rid of the stuff you don’t need? By turning it into pee!
Wow! Look at these arm muscles!
Muscles make you strong and help you move.
But muscles are not so strong with crystals in them.
Help Ruby find a crystal.
Guess what? There are muscles all over your body—even in your throat where they help you swallow!
Ruby has crawled into the lungs. They are in your chest.
Your lungs breathe for you. They take air in and push it out of your body so your body can make energy.
The lungs also help you talk and SHOUT!
But the lungs may have some trouble working if there are crystals in them.
Are there any crystals here for Ruby to find?
Next stop, the brain!
But wait. Ruby sees something that looks like a butterfly. It’s in the neck.
It’s the thyroid. It helps your body work normally so you can grow!
But it can’t help you grow with crystals in it.
Ruby better stop and find a crystal. Can you help?
Can you guess where Ruby is now?
In the amazing brain!
The brain lets you think and feel things.
Help Ruby find a crystal so the brain can think well.
Look! Can you see where Ruby is now?
She’s in the eyes. Your eyes see the world.
But—you already know—the eyes can’t see like they should with crystals in them.
Help Ruby find a crystal.
And if you find sunglasses, give them to Ruby. It’s bright in here!
You did it!
You helped Ruby find all the crystals!
Ruby is done with her job for now. She will make another trip through the body later. She tells her friends that it's their turn.
“Get going, guys!” Ruby says. “We’ve got to keep this kid as healthy as we can!”
This activity book is filled with fun things for kids to do while they read and learn what it’s like for Michael to live with cystinosis. It’s a great way to start a conversation with children to help them understand cystinosis.
Start the discussion now with these downloadable coloring pages! Then keep the conversation going for years to come with a bound copy of Michael’s Show-and-Tell Activity Book.
You can check how much you and your child have learned by taking a fun interactive quiz.
Watch this animated video about siblings Michael and Andrew. Michael has cystinosis and is not feeling well enough to attend Andrew’s dress rehearsal for his piano recital. See how the entire family works together to manage disappointment and take care of each other.
[BACKGROUND MUSIC] Piano – a familiar tune, but played more slowly than usual, like a beginner is practicing. The music stops briefly, then starts again. Same song.
[MOM] Do you think you can make it to Andrew’s dress rehearsal?
[MICHAEL] I don’t think I can, mom. I feel sick.
AUDIO: Piano, stops
[MOM] Michael isn’t feeling well. We won’t be able to make the rehearsal.
[ANDREW] But you missed the last one!
[AUDIO] Piano, loud
[MOM] Andrew!
[MOM] I know the timing is terrible, but you know Michael has good days and bad. We’ll be there for the recital.
[ANDREW] Sometimes I wish I was sick too.
[MOM] Andrew is pretty upset, but Samira’s mother is going to pick him up and take him.
[MICHAEL] I hate being sick and causing problems…
[MOM] It’s not your fault, Michael.
[FRIEND] Where’s your family?
[ANDREW] My brother is not feeling well today so they couldn’t make it.
[MICHAEL] That’s a strike!
[MICHAEL] Hey, that’s my jacket!
[MUSIC] Piano continues. An off-key piano note or two interrupts the flow of the song.
[MICHAEL] I’m sorry I wasn’t feeling good and missed your dress rehearsal.
[ANDREW] It’s ok. I’m used to it.
[MICHAEL] I’d like to make it up to you with a song.
[MOM] You were awesome tonight, Andrew.
[ANDREW] How would you know?
[MOM] Samira’s mom sent me a video of your performance.
[ANDREW] That’s not the same as being there.
[MOM] I know.
[MOM] Would you mind playing your song now?
[ANDREW] Well. I am a little tired. But Ok.
[Piano] Same song, taken from the top
©2023 HORIZON THERAPEUTICS PLC DA-UNBR-US-01279 04/23
Michael is a 12-year-old boy living with cystinosis. Andrew is his brother and best friend. Read this animated comic to see how the entire family works together when Michael is not feeling well enough to attend Andrew’s dress rehearsal for his piano recital. It also includes some fun activities and a guide for discussion.
Have your child provide this handout to their teachers to help the staff better understand cystinosis and support your child’s needs.

Sometimes medical terms can be tough to understand. But learning the words used to talk about cystinosis may help you be clear with doctors, family, and friends. This glossary is a great place to start.
Amino acid: A building block of proteins used in every cell to help the body grow.
Cystine: The amino acid that builds up inside of cells when a person has cystinosis.
Cystine-depleting therapy (CDT): A treatment that works to reduce the buildup of cystine in cells. Learn how taking a CDT as prescribed may help keep cystine levels low around the clock.
Cystine level test: A blood test that measures the amount of cystine in white blood cells at a given time. There are two tests that can measure cystine levels: mixed leukocytes and granulocytes.
Dialysis: A medical treatment to clean the blood when the kidneys do not work as they should.
Fanconi syndrome: A kidney disorder that causes the body to lose important substances needed for good health. It causes extreme thirst and frequent peeing (urination).
Granulocyte: A type of white blood cell that is collected in a blood sample during cystine level testing.
Hypothyroidism: A condition in which the thyroid gland is unable to make enough thyroid hormone, causing the body to not work like it should. Common symptoms include, but are not limited to, slowed growth, tiredness, and weight gain.
Immune system: A group of cells that protect the body against attacks by germs.
Infertility: Inability to cause pregnancy (for men) or inability to get pregnant (for women). Women of childbearing age with cystinosis may become pregnant.
Kidney transplant: A surgery to place a healthy kidney from a donor into the body of a person with failing kidneys.
Leukocytes: Commonly referred to as white blood cells; a collection of cells that help the body fight infections. One of the two available cystine level tests collects leukocytes in a blood sample.
Lysosome: The part of a cell that acts as a “recycling center” by breaking down proteins into amino acids. This is the part of the cell where cystine becomes trapped and builds up in people with cystinosis.
Myopathy: A disease that affects the muscles, making a person feel very weak.
Nephropathic cystinosis: Cystinosis of the kidney; often called classic infantile cystinosis because its symptoms usually appear within a child's first year of life. This is the most common (95% of all cases) and most severe form of cystinosis.
Photophobia: In patients with cystinosis, a buildup of cystine in the eyes may result in light sensitivity, or the eye's inability to tolerate light. It may also cause eye pain and severe headaches.
Rickets: Softening and weakening of bones in children, usually caused by a lack of vitamin D (phosphate) in the body.
White blood cells (WBCs): Also called leukocytes; a collection of cells that help the body fight infections.

You are not alone. The resources below may help you meet others living with cystinosis, learn about advocacy programs, explain what cystinosis is, and much more.
Global Genes is a nonprofit advocacy organization for patients and families fighting rare and genetic diseases, including cystinosis. Its mission is to eliminate the challenges of rare disease.
An independent kidney patient organization, AAKP is dedicated to improving the lives and outcomes of kidney patients through education, advocacy, patient engagement, and patient communities.
Learn moreCRF supports research that aims to improve the quality of life of patients with cystinosis, find better treatments, and ultimately find a cure.
Learn moreDPC is a patient-led, nonprofit organization dedicated to improving dialysis patients’ quality of life by advocating for favorable public policy.
Miracle Flights is a nonprofit health and welfare organization providing financial assistance for medical flights so that seriously ill children may receive life-altering, life-saving medical care and second opinions from experts and specialists throughout the United States.
CRN is an all-volunteer, nonprofit organization dedicated to supporting and advocating for research, providing family assistance, and educating the public and medical communities about cystinosis.
The Cystinosis Foundation of New Jersey is a nonprofit advocacy organization devoted to increasing awareness of cystinosis and funding medical research related to treating and curing those with the condition.
AKF is a nonprofit organization serving the millions of Americans with kidney disease. American Kidney Fund helps people fight kidney disease and live healthier lives by providing a wide range of programs and services, including prevention activities, educational resources, and financial assistance.
Learn moreDiscover the many ways Amgen has supported people with cystinosis in Committed to the Cystinosis Community.